SOAP note
The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by health care providers to write out notes in a patient's chart, along with other common formats, such as the admission note.
Full Answer
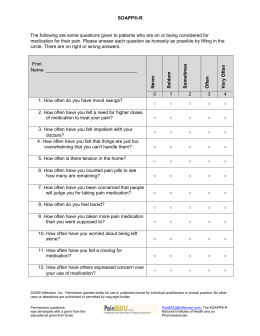
What is a SOAP note for mental health?
The sample SOAP note acronym offers a clever way to thoroughly address the emerging situation of a patient. While physical information does not always require to be provided in the SOAP note format for mental treatment, the SOAP note template can be useful to therapists if they coordinate treatment with another health professional’s client.
How do you List A patient’s complaint on a SOAP note?
See what their Chief Complaint (CC) is and list that at the top of your SOAP note. The CC will help other medical professionals see what the patient’s condition is so they know what to expect from the rest of the note.
How to document a patient assessment (soap)?
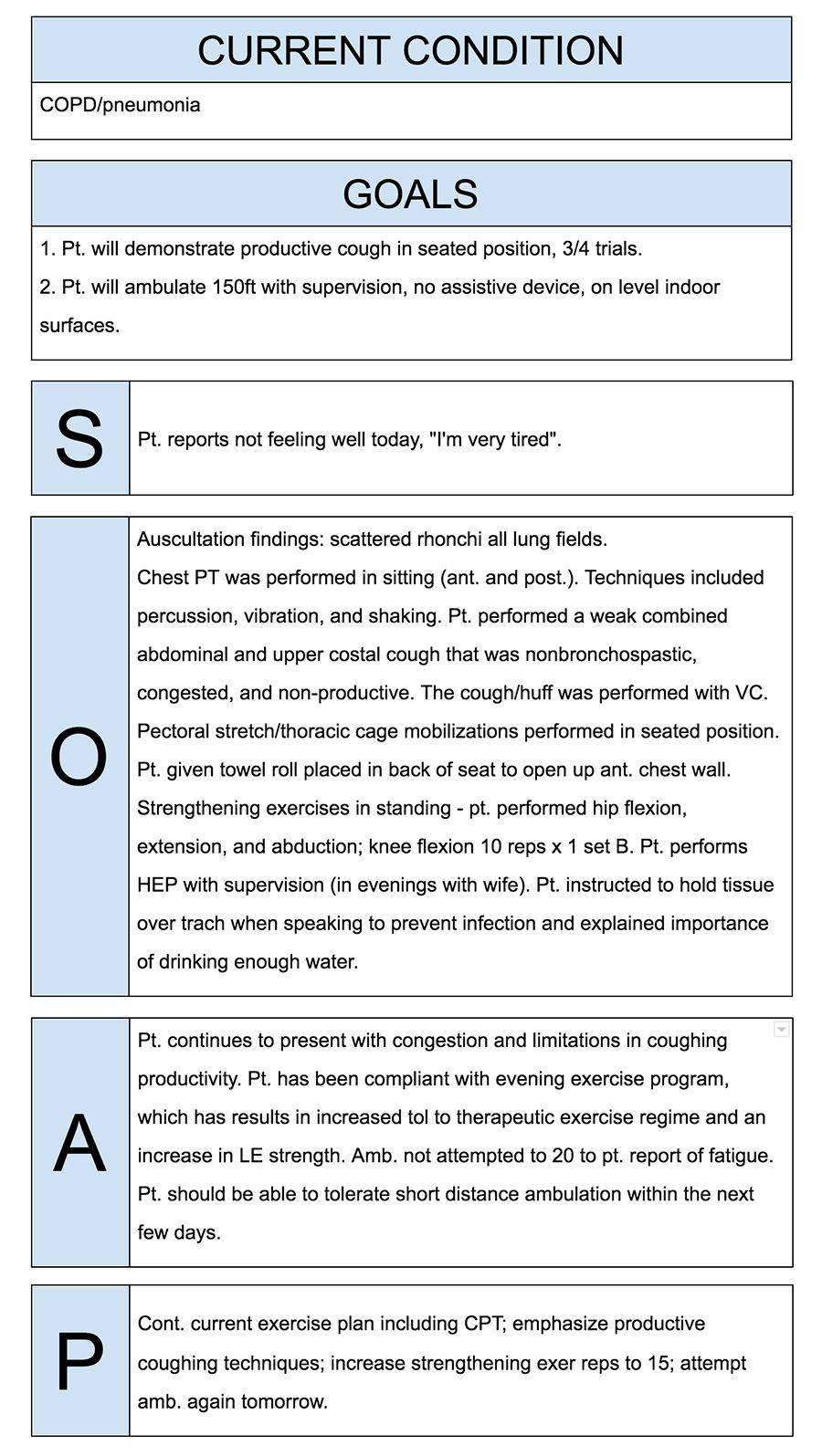
How to Document a Patient Assessment (SOAP) 1 Subjective. The subjective section of your documentation should include how... 2 Objective. This section needs to include your objective observations,... 3 Assessment. The assessment section is where you write your thoughts on the salient issues and... 4 Plan. The final section is the plan,...
What is SOAP note format in nursing?
Writing in a SOAP note format—Subjective, Objective, Assessment, Plan—allows healthcare practitioners to conduct clear and concise documentation of patient information. This method of documentation helps the involved practitioner get a better overview and understanding of the patient’s concerns and needs.
What does soap mean in medical records?
Subjective, Objective, Assessment and PlanIntroduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers.
How do you write a soap report?
Tips for Effective SOAP NotesFind the appropriate time to write SOAP notes.Maintain a professional voice.Avoid overly wordy phrasing.Avoid biased overly positive or negative phrasing.Be specific and concise.Avoid overly subjective statement without evidence.Avoid pronoun confusion.Be accurate but nonjudgmental.
What is included in a SOAP note?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What is soap format of assessment?
The Subjective, Objective, Assessment and Plan (SOAP) is an acronym representing a widely-used method of. documentation in veterinary and human medicine. The SOAP is a way for healthcare workers to document their. thinking in a structured and organized way.[1][2][3]
What are the 4 parts of soap?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan.
What is a good SOAP note?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
What is the purpose of a SOAP note?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
How do you write a SOAP note in nursing?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
How long should a SOAP note be?
1-2 pagesYour SOAP notes should be no more than 1-2 pages long for each session. A given section will probably have 1-2 paragraphs in all (up to 3 when absolutely necessary).
How do you review a patient?
Reviewing patients on callThe importance of reviewing patients. ... Ask for the basics while youre on your way. ... Make a rapid initial assessment. ... Look at the observations chart. ... Review the notes. ... Take a focused history. ... A full and formal examination. ... Putting it all together.More items...•
How do you document patient history?
How To Properly Document Patient Medical History In A ChartPresenting complaint and history of presenting complaint, including tests, treatment and referrals.Past medical history – diseases and illnesses treated in the past.Past surgical history – operations undergone including complications and/or trauma.More items...•
How do you write a SOAP note for physical therapy?
Now that you have a general idea of what a SOAP note consists of, let's take a more detailed look at each section....These “Problem-orientated medical records (POMR)” included details about:The patient's specific problems.The therapist's desired outcomes.A diagnosis if applicable.Treatment plan details.
What are 3 guidelines to follow when writing SOAP notes?
4 tips for writing SOAP notes Don't repeat content from a previous section. Make sure each section has unique content. Don't rewrite your whole treatment plan each time.
How do you write a nursing SOAP note?
0:105:59How to Make SOAP Notes Easy (NCLEX RN Review) - YouTubeYouTubeStart of suggested clipEnd of suggested clipUse the soap note as a documentation method to write out notes in the patient's chart. So stands forMoreUse the soap note as a documentation method to write out notes in the patient's chart. So stands for subjective objective assessment and plan let's take a look at each of the four components.
How do nurse practitioners write SOAP notes?
9:2229:55HOW TO WRITE A SOAP NOTE / Writing Nurse Practitioner Notes ...YouTubeStart of suggested clipEnd of suggested clipQuestion mark um less exercise. Question mark anything else you want to ask them about it write theMoreQuestion mark um less exercise. Question mark anything else you want to ask them about it write the question out there so all you have to write is like yes or no when you're actually in the room.
How long should a SOAP note be?
1-2 pagesYour SOAP notes should be no more than 1-2 pages long for each session. A given section will probably have 1-2 paragraphs in all (up to 3 when absolutely necessary).
What are the four parts of a SOAP note?
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan which is the four parts of a SOAP note . All four parts are designed to hel...
Are SOAP notes still used?
Yes, It is still widely being used in modern clinical practice. Whether in paper or digital format, a soap note is one of the tools used by healthc...
What is the advantage of using a SOAP note?
SOAP note helps in providing succinct yet thorough and relevant medical information about the patient. Other benefits include: It makes tracking o...
Why do nurses write soap notes?
It is very beneficial to write down notes to keep track of and record the progress of treatments of patients.
What is a soap note?
SOAP notes are a type of documentation which, when used, help generate an organized and standard method for documenting any patient data. Any type of health professionals can use a SOAP note template – nurse practitioners, nurses, counselors, physicians, and of course, doctors. Using these kinds of notes allows the main health care provider ...
Why are soap notes still used?
SOAP notes have been around for some time now and because of their efficiency and functionality, they are still being used now. The very first SOAP note template was created and developed by a brilliant doctor named Lawrence Weed way back in the 1960s. It was done at the University of Vermont as an element of the POMR (Problem-Oriented Medical Record). During those times, objective documentation did not exist so physicians had the tendency to make decisions about treating patients without scientific basis.
What is a soap note template?
A SOAP note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. A SOAP note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
Why do you write a note after a patient is treated?
After you’ve administered treatment to a patient, writing a note about it would inform other physicians that you were able to competently help the patient. On the side of the patient and the family as well, you’d have concrete proof to show them in case they have any questions about the treatment.
What are some examples of factors that affect the quality of a patient?
Some examples of this would be if the patient felt better after taking certain medicines if the patient feels better or worse when in certain positions and other such factors.
Why is it important to have a patient's notes?
Having these notes would prove that there had been regular patient contact throughout the whole treatment period and the stay of the patient in the hospital.
What is a soap note?
A SOAP note is a documentation method used by medical practitioners to assess a patient’s condition. It is commonly used by doctors, nurses, pharmacists, therapists, and other healthcare practitioners to gather and share patient information. SOAP notes are designed to improve the quality and continuity of patient care by enhancing communication ...
What are the Four Parts of a SOAP Note?
The four parts of a SOAP note are the same as its abbreviation. All four parts are designed to help improve evaluations and standardize documentation:
What is the best software to collect SOAP notes?
Healthcare professionals can use iAuditor, the world’s #1 inspection software, to digitally gather SOAP notes and improve the quality and continuity of patient care. Collect photo evidence for a more informative and descriptive patient record.
Can iAuditor save patient records?
Easily share your findings with other healthcare clinicians and avoid losing track of patient records by securely saving it in the cloud using iAuditor
Can you download soap note templates?
To help you get started we have created SOAP note templates you can download and customize for free.
What is a SOAP note?
The SOAP note is a way for healthcare workers to document in a structured and organized way .[1][2][3] The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers.
What is a comprehensive soap note?
A comprehensive SOAP note has to take into account all subjective and objective information, and accurately assess it to create the patient-specific assessment and plan.
What are the headings of a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan. Each heading is described below.
Why is a soap note important?
The advantage of a SOAP note is to organize this information such that it is located in easy to find places.
Why do we use soap notes?
It also provides a cognitive framework for clinical reasoning. The SOAP note helps guide healthcare workers use their clinical reasoning to assess, diagnose, and treat a patient based on the information provided by them.
What is the opening statement for HPI?
The HPI begins with a simple one line opening statement including the patient's age, sex and reason for the visit. Example: 47-year old female presenting with abdominal pain. This is the section where the patient can elaborate on their chief complaint. An acronym often used to organize the HPI is termed “OLDCARTS”:
SOAP note example for Nurse or Nurse Practitioner
John reports that he is feeling 'tired' and that he 'can't seem to get out of bed in the morning.' John is 'struggling to get to work' and says that he 'constantly finds his mind wondering to negative thoughts.' John stated that his sleep had been broken and he does not wake feeling rested.
SOAP note example for Psychotherapist
Stacey reports that she is 'feeling good' and enjoying her time away. Stacey reports she has been compliant with her medication and using her meditation app whenever she feels her anxiety.
SOAP note example for Paediatrician
Mrs. Jones states that Julia is "doing okay." Mrs. Jones said her daughter seems to be engaging with other children in her class. Mrs. Jones said Julia is still struggling to get to sleep and that "she may need to recommence the magnesium." Despite this, Mrs. Jones states she is "not too concerned about Julia's depressive symptomology.
SOAP note example for Social Worker
Martin has had several setbacks, and his condition has worsened. Martin reports that the depressive symptoms continue to worsen for him. He feels that they are 'more frequent and more intense. Depressive symptomology is chronically present.
SOAP note example for Psychiatrist
Ms. M. states that she is "doing okay." Ms. M. states that her depressive symptomatology has improved slightly; she still feels perpetually "sad." Ms. M.
SOAP note example for Therapist
"I'm tired of being overlooked for promotions. I don't know how to make them see what I can do." Frasier's chief complaint is feeling "misunderstood" by her colleagues.
SOAP note example for Counselor
David states that he continues to experience cravings for heroin. He desperately wants to drop out of his methadone program and revert to what he was doing.
Why do healthcare workers use SOAP notes?
Healthcare workers use Subjective, Objective, Assessment, and Plan (SOAP) notes to relay helpful and organized information about patients between professionals. SOAP notes get passed along to multiple people, so be clear and concise while you write them. By listing accurate information and informed diagnoses, you can help a patient get the best care!
What is the objective section of a soap note?
The Objective section of the SOAP note refers to data that you collect and measure from the patient.
How many testimonials does wikihow have?
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 14 testimonials and 93% of readers who voted found it helpful, earning it our reader-approved status.
Why do we use soap notes?
SOAP notes are especially helpful for sharing information between different providers who are treating the same patient.
What is subjective in soap notes?
The Subjective section of your soap note is about what the patient is experiencing and how they are handling their concerns. Some common examples may include chest pain, decreased appetite, and shortness of breath. You can also talk to a family member or spouse to get any necessary information.
How to write down a medication?
Write down any therapy or medications the patient should try. If you believe that the patient needs rehabilitation , such as physical or mental therapy, be sure to list any that can apply. If a prescription medication is more appropriate, then write the type of medication, the dosage, and how long they should take it .
How to write down a physical exam?
Write down any information you gather from a physical exam. Assess the area that the patient is concerned about so you can write down detailed observations about it. Avoid writing the symptom that the patient is feeling; instead, look for objective signs while you’re performing the physical. Keep your notes clear and organized so they aren’t confusing to anyone else reading them. [6]
What can a physician use the information contained in a soap note?
The physician can use the information contained in the SOAP note to set the steps for relevant diagnostic procedures for the patient. From the information in the SOAP note, they may recommend the patient to another specialist for further observations.
What do you write in a soap note?
The SOAP note format helps medical professionals to record patient data easily through a highly structured style. This highly structured style often enables workers to easily find patient records and, when needed, retrieve key information
What should a SOAP plan include?
With each diagnosis, the SOAP plan format should include measurable objects. If your patient experiences several symptoms in tandem with a drug use disorder, such as post-traumatic stress disorder, your findings must contain distinct measures for each diagnosis.
Do you need to provide a soap note for mental health?
While physical information does not always require to be provided in the SOAP note format for mental treatment, the SOAP note template can be useful to therapists if they coordinate treatment with another health professional’s client.
Can you record your observations on a soap note?
Based on the information you’ve obtained, you can record your observations and make conclusions. For first visits, an assessment centered on the nature and magnitude of symptoms identified and signs witnessed could or could not be included in the evaluation section of your soap note format.
