What is a nursing report sheet?
When a patient has been registered for care in a healthcare institution, nurses form to be one of the primary groups in-charge of taking care of the said patients. In order to make sure that they are able to provide the optimum required care, nurses use a tool known as the Nursing Report Sheet.
Why are shift report sheets important in nursing?
They are often viewed as a crucial entity that helps them to pass on patient information during routine changes in the shifts of nurses. Shift report sheets are highly useful in providing adequate information transfer, thus increasing communication levels between the nurses.
What is completion in a nursing report template?
Completion – Completion is the final section of a nursing report template. This section contains the details regarding the nurse on duty. The various details to be recorded here are the Name, Signature of the Nurse and the Date and Time of the ending of the shift.
What is the first section of a nursing report?
General Information – The General Information section is the first section to be present in the Nursing Report. This section is responsible for generating all the details regarding the patient such as Date of Birth, Gender etc. of the patient. Patient Report – Next on the report, is the Patient Report section.

What is a report sheet in nursing?
Nursing report sheets (also known as patient report sheets or nursing brain sheets) are templates nurses fill out with important patient information. These sheets are handoffs at the end of each shift and are given to the new nurse taking over for the next shift.
What should be included in a nurse to nurse report?
What to cover in your nurse-to-nurse handoff reportThe patient's name and age.The patient's code status.Any isolation precautions.The patient's admitting diagnosis, including the most relevant parts of their history and other diagnoses.Important or abnormal findings for all body systems:More items...•
How do you write a nursing assessment report?
How to write a Nursing Assessment Report: A Step by step GuideCollect Information. ... Focused assessment. ... Analyze the patient's information. ... Comment on your sources of information. ... Decide on the patient issues.
Why is report so important in nursing?
Recording nursing reports plays a vital role in the coordination between treatment team members, continuity of care and nurses' partnership in professional duty and responsibilities, intervention's evaluation, determining nursing care expenses and protecting patients' and nurses' rights.
What are the 5 P's of patient handoff?
The Sentara health care organization adopted behavior-based expectations to improve the handoff process and used tools including the five Ps (patient/project, plan, purpose, problems, and precautions). It reported a 21-percent increase in effective handoffs.
How do I write a nursing report daily?
How to write a nursing progress noteGather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. ... Record objective information. ... Record your assessment. ... Detail a care plan. ... Include your interventions.
How do you write a patient report?
Summary: The format of a patient case report encompasses the following five sections: an abstract, an introduction and objective that contain a literature review, a description of the case report, a discussion that includes a detailed explanation of the literature review, a summary of the case, and a conclusion.
What are the 4 types of nursing assessments?
The four medical assessments regularly performed on patients are:Initial assessment. ... Focused assessment. ... Time-lapsed assessment. ... Emergency assessment.
What are the 5 legal requirements for nursing documentation?
The documentation needs to be concise, legible, and clear. There must be accurate information about the actions taken, assessments, treatment outcomes, complications, risks, reassessment processes in treatments, and changes in the treatment.
What are the types of reports in nursing?
There are different types of nursing reports described in the literature, but the four main types are: a written report, a tape-recorded report, a verbal face-to-face report conducted in a private setting, and face-to-face bedside handoff.
What is the most common incident reported in hospitals?
Medication-related incidentsMedication-related incidents are the most commonly reported incidents in healthcare.
What is the last thing you should do before sending a report?
What is the last thing you should do before sending a report? Proofread it. Ask another security officer or supervisor to read it and look for errors.
What should a handoff report include?
Nurses complete their handoff report with evaluations of the patient's response to nursing and medical interventions, the effectiveness of the patient-care plan, and the goals and outcomes for the patient. This category also includes evaluation of the patient's response to care, such as progress toward goals.
What are the 5 legal requirements for nursing documentation?
The documentation needs to be concise, legible, and clear. There must be accurate information about the actions taken, assessments, treatment outcomes, complications, risks, reassessment processes in treatments, and changes in the treatment.
What is documentation and nursing report?
Documentation is anything written or printed that is relied on as a record of proof for authorized persons. Documentation and reporting in nursing are needed for continuity of care it is also a legal requirement showing the nursing care performed or not performed by a nurse.
What should CNA report to nurse?
Other circumstances that require immediate reporting: skin changes, falls, patient complaints, difficult behavior, suicidal or dangerous behavior, and discovery of alcohol or drugs. The CNA should also report if the patient refuses to eat or cooperate with care.
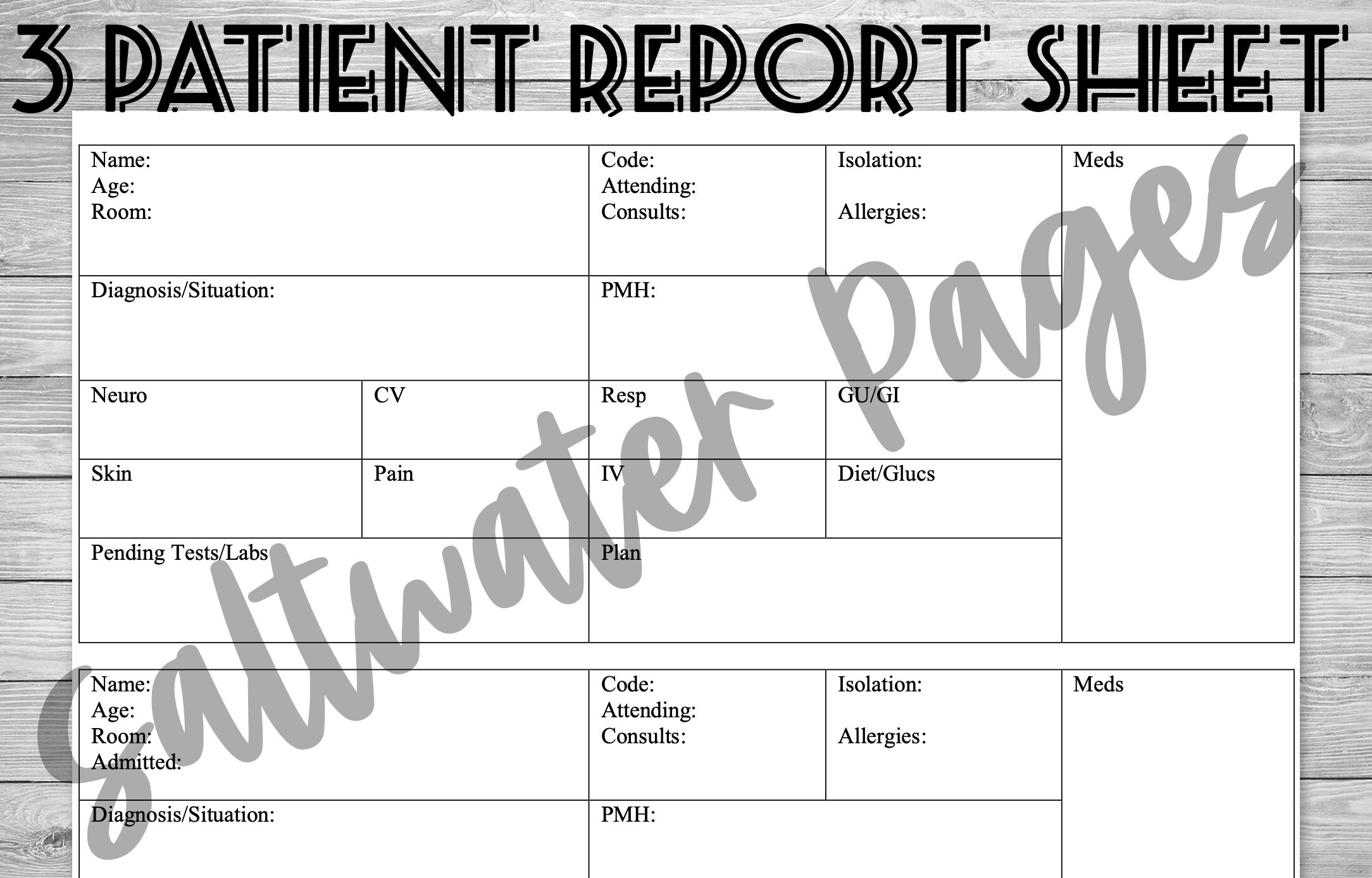
What is a nursing report sheet?
Nursing report sheets are premade templates of paper used by nurses to help them keep track of their patients. A nursing report sheet is started at the beginning of the nurses shift while she/he is getting report from the leaving nurse who is giving them nursing report.
Why Do Nurses Use Nursing Report Sheets?
Nurse report sheets are very handy because they contain tidbits of vital information concerning your patient’s diagnosis, history, allergies, attending doctor,consults, things that need to be done on your shift, medication times, vital signs, lab results etc. The report sheet has other usage as well. Other usages of the nursing report sheet include but are not limited to:
What is a nursing note?
Nursing notes to remind yourself of things you need to do for the patient or chart on. Notes to yourself on things you want to remind the next shift. Most nurses who use report sheets consider their report sheet to be their “brain,” and panic when they misplace them.
Why is it important to have a 6 to 7 patient load?
When you have a 6 to 7 patient load, patient diagnosis and histories can run together and you may get them confused. Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do.
How to find out a patient's INR?
Fast access to patient information. If you are asked by a doctor what a particular patient’s INR was you could simply look at your report sheet to find out. You won’t have fumble around and try to remember which patient he/she was talking about.
Why do you write down on your chart sheet?
Helps you keep your charting more accurate. If you write down on your report sheet things you need to remember to chart, your charting will be more accurate and easier to do. Again with 6 to 7 patients things tend to run together.
Can you print a report sheet for nurses?
You can share them with other nurses as well. Simply click the picture of the report sheet you like and after you download it you can print them. Tip: for less report sheets to carry around set your printer settings so you can print on the back side.
What are Nursing Report Sheets?
Nursing report sheets (also known as patient report sheets or nursing brain sheets) are templates nurses fill out with important patient information.
Take the Next Steps to Become a Nurse
Staying organized as a nurse is vital to keeping your patient happy and healthy. A nursing report sheet serves as the blueprint for everything someone would want to know about your patient – and you’ll find a lot of the elements above on many templates regardless of which nursing specialty you choose.
What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
You Need a Nursing Brain Sheet That Works for YOU
For the longest time, I have tried pushing the brain sheet that worked for me onto new students and newbie nurses. I’ve changed my tone.
The Nursing Brain Sheet Database
The response was AMAZING (to say the least). We received over 100 report sheet templates from nurses working in MedSurg, ICU, ED, OB, Peds, Tele . . . you name it.
1. Handoff and Nursing Report Sheet
This is the report sheet that my preceptor used to make me fill out prior to the end of each shift as a newbie. To be honest, at first, I was so annoyed that I had to spend like an hour at the end of each shift filling this out. It wasn’t until I realized I was able to give a badass report that I was finally grateful she made me fill this out.
3. 4 Patient Simple Tele Sheet
Some people like it simple . . .this is the sheet for you. With slight prompting, this sheet makes a great tool for the MedSurg or Tele nurse on the GO!
4. 4 Patient Simple Nurse Task Sheet
I love this one. At first glance it looks basic . . . but at closer inspection, you start to see all the details and information you have available with it. From lab values to foley care, to last pain med, this is would be a great one for a nurse that has a flow and just wants a simple push to stay a bit more organized.
5. Vertical Nurse Brain sheet with Assessment Diagram
I’m a visual learner. This one just grabs my attention. I like the top section for the “essentials” like blood sugars, DX, and Pt info. I also really like the area below the charts to draw little notes about your physical assessment. I really like this nursing brain sheet for beginner or experienced nurses.
What is an organization sheet in med sg?
What a Med Surg organization sheet contains? At the Med Surg department, there are certainly organization sheets that are part of their duties. Contains data about patients in the scope of their care. For example, the room where the patient was treated, the name of the patient, the contact of the person closest to the patient, ...
How to get a medical surg organization sheet?
To get a Med Surg legal organization sheet, you must become a medical Surg nurse. If you are studying that ends in the Med Surg department, you will find it in the learning syllabus provided. But if you are just an ordinary person who just wants to know the contents of the Med Surg organization sheet, you can find references for example from the internet. But for the record, it will be a criminal offense if you use it for important needs or validation but in reality, do not get treatment from med surg nurse because you are healthy.
Why is the knowledge possessed by each nurse so different?
The knowledge possessed by each nurse is very different because, in their studies, they have focused on one department. So that the action that can be taken by all the nurses initially is general medical knowledge.
What is the Med Surg department?
Med Surg stands for medical-surgical which is a department that contains nurses specifically handling patients who need recovery after undergoing surgery. There is no specific age for patients treated by Med Surg nurses. To be sure, after undergoing surgery, patients will find it difficult to move the body and there are even some patients who need to get extra attention, this is what the department stands for.
